The Intake - Refining and Building the Client Case
The Intake – Adding to our Intake
When we are adding to the intake form, there is no need to increase your questionnaire, although you can of you want.
The 10 questions were traditionally used verbally so that the practitioner could observe the reactions of the client while they record, as the reaction is as important as the response.
Your client may never have had such in depth questioning, so be prepared to explain that you are working on a more in depth analysis that will assist your treatment outcomes.
Record their answers, you can always look back later while you are doing your review of findings and journal on any changes in your perception and approach to the treatment.
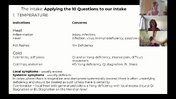
Using the 10 Questions in our Intake
When we are adding to the intake form, there is no need to increase your questionnaire, although you can of you want.
The 10 questions were traditionally used verbally so that the practitioner could observe the reactions of the client while they record, as the reaction is as important as the response.
Your client may never have had such in depth questioning, so be prepared to explain that you are working on a more in-depth analysis that will assist your treatment outcomes.
Record their answers, you can always look back later while you are doing your review of findings and journal on any changes in your perception and approach to the treatment.
Using the 10 Questions in our Intake
The key here is to identify repeating patterns, words descriptions to form an accurate assessment
1.Temperature
What is your favourite temperature?
What is your favourite season?
Do you get cold easily?
Do you catch a cold easily?
- Sweat
Do you sweat easily?
Do you ever notice an odour when you sweat?
Do you ever sweat when you shouldn’t, or not sweat when you should?
3. Head and Face
Do you suffer from Headaches?
What part of the head?
Would you describe the pain as fullness, throbbing, stabbing, deep, dull?
Rate 1-10
Do you have tinnitus?
Location? One side or both?
What is the tone? (high pitch, low pitch, loud, quiet, varied at times of the day)
Do you have sinusitis? Allergies? When?
Eye problems? (floaters, fatigue, pain or vision changes)
Teeth or jaw issues? (TMJ, lots of dental work)
- Pain
Location of Pain (list each separately)
How long has the pain been there?
Have you had this pain before?
Do you know what caused the pain?
Frequency of pain daily, weekly monthly
Time of Day (getting up in am, with movement, end of day)
Pain Scale 1-10
Acute or Chronic
Describe the pain: Stabbing, Throbbing, Distending, Burning, Heavy, Sharp, Dull, Tingling, Shooting, Numbness
- Urine/Stool
How many times do you urinate per day?
Nighttime urination?
Colour of urine?
Smell?
How many bowel movements do you have per day? (normal 1-3)
Are bm easy to pass?
Does it ever vary in texture and appearance?
Colour? (should be rich brown)
Undigested food?
Alternating constipation and diahhrea?
- Thirst, Appetite, Taste
Thirst – How much do your drink?
Do you prefer cold-warm-hot beverages?
Types of beverages coffee / alcohol consumption / juice
Appetite – How much do you eat?
How often do you eat?
What times of the day do you eat?
Favourite foods / flavour
Aversions to foods / smells / textures
Allergies or food aversions
- Sleep
How is your sleep?
Quality of sleep?
How many hours do you sleep per night?
How many hours of sleep do you need?
Do you go to bed and wake at the same time?
Do you sleep well?
Wake rested?
Wake at the same time each night?
- Thorax / Abdomen
Any discomfort in the abdomen?
Digestive problems?
Time of day?
Location?
Type of pain?
Relieved by?
Triggered by?
- Gyneological
At what age did period start?
Length of cycle? 28 days Length of actual period
Colour of Blood? Clots?
Changes over time?
Symptoms occur: before during after
Symptoms: Pain (type: cramping, stabbing, dull, deep)
Location (back, abdomen, legs head etc)
Relieved with pressure, exacerbated with pressure
Emotions, Headaches, Focus,
- Health History

















0 comments
Leave a comment